How to Manage a Privacy Breach in Your Canadian Practice
How to Manage a Privacy Breach in Your Canadian Practice Workshop
Have you ever heard about a privacy breach at another practice and thought…
“I hope that never happens to us.”
The reality is — privacy breaches can happen in any healthcare practice, regardless of size, specialty, or technology. Whether it’s a misdirected fax, unauthorized access to a chart, lost device, or cyber incident, breaches are not a matter of if — but when.
What makes the difference is how prepared you are to respond.
I’m tickled pink to partner with Kayla Das to deliver a live virtual workshop designed to provide practical, step-by-step guidance for Canadian healthcare practices. Kayla Das B.Rec, BSW, MSW, RSW is a trusted Business Coach For Therapists and Counsellors.
Live Virtual Workshop
How to Manage a Privacy Breach in Your Canadian Practice
In this interactive on-line session, we’ll walk you through what to do when a privacy breach occurs — before you ever have to face one in real time.
This workshop is ideal for:
- Canadian clinic managers
- Privacy officers
- Practice owners
- Social workers, counsellors, and mental health leaders
- Clinical supervisors and consultants
If you are responsible for protecting patient information, this training will help you strengthen your breach response readiness.
What We’ll Cover
Participants will learn:
- The difference — and overlap — between confidentiality and privacy
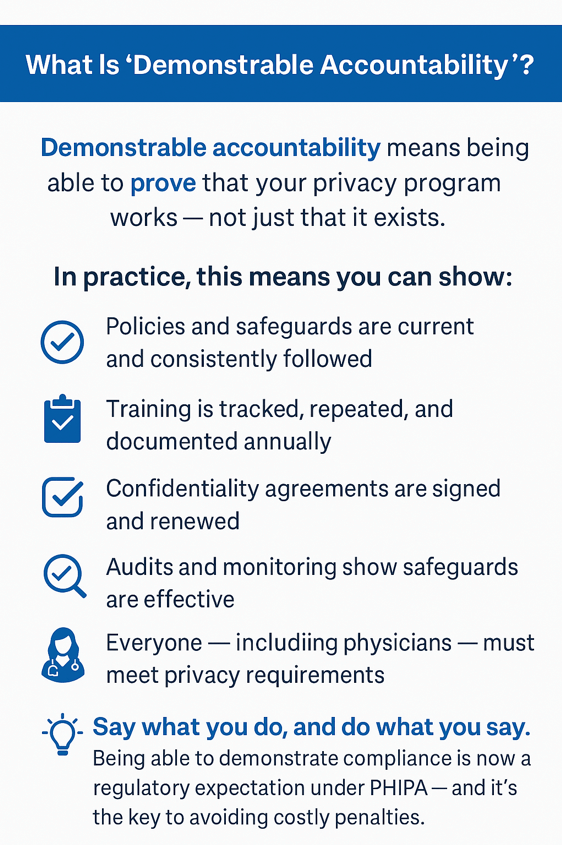
- Legislative, regulatory, and professional practice requirements across Canada
- Why privacy breaches are a significant risk you should prepare for
- How to recognize when a breach has occurred
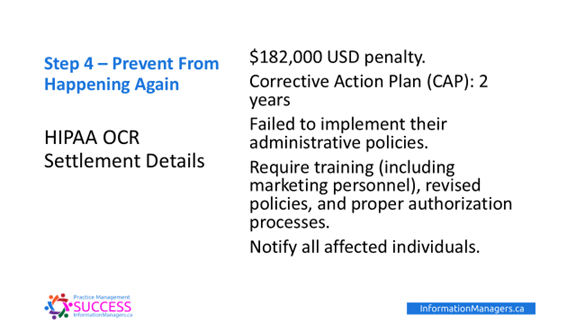
- The 4-Step Response Plan for managing a privacy breach
- Practical steps to prevent breaches before they happen
… and more
Important for Ontario Practitioners
Ontario health information custodians (practice owners) are required to submit annual privacy breach statistics to the Ontario Information and Privacy Commissioner by March 1 each year.
If you’re unsure what must be reported — or how to prepare — this workshop will address those requirements.
Workshop Details
Date: Tuesday February 24, 2026
Time: 9:00 AM PST / 12:00 PM EST / 10 AM MT
Length: Approximately 90 minutes
- Presentation: 45–60 minutes
- Live Q&A: Up to 30 minutes
- $75 CAD + tax
Click HERE to Save Your Seat!
Bonus Benefits
✔️ Replay access available until March 10, 2026
✔️ Certificate of Attendance available for live participants (may support continuing education credits)
Privacy breaches are stressful — but managing them doesn’t have to be overwhelming when you have a plan.
We hope you’ll join us for this practical, supportive session designed to help you protect your patients, your practice, and your professional reputation.