Why “Demonstrable Accountability” Matters
Why “Demonstrable Accountability” Matters
Does Your Privacy Program Have ‘Demonstrable Accountability’?
The first Ontario decision to include an Administrative Monetary Penalty (AMP) under the Personal Health Information Protection Act (PHIPA) shows how serious the consequences can be when personal health information (PHI) is used for an unauthorized secondary purpose.
Privacy Breach Nuggets takes real cases and turns them into practical lessons for privacy officers, clinics, and healthcare practices. Let’s dive into what went wrong, what worked, and how you can apply these insights to strengthen your privacy program.
What Happened
This case includes the Windsor Regional Hospital, Chatham-Kent Hospital Alliance, Erie Shores Healthcare, WE Kidz Pediatrics, and Dr. Omar Afandi.
Between April 20 and May 7, 2024, Dr. Afandi accessed the shared electronic health record (EHR) system of CKHA’s Women’s and Children’s Program. He used it to identify newborns so he could contact their parents to offer circumcision services at his private practice, WE Kidz Pediatrics.
Several parents reported receiving these unsolicited calls and complained to the hospitals. Dr. Afandi later stated he did not realize these accesses were unauthorized under PHIPA.
Managing the Breach
We can analyze the hospitals’ and clinic’s response using the 4-Step Response Plan.
Step 1 – Spot and Stop
The breach was reported by patients who received unsolicited contact from the physician.
The Chief of Staff wrote to Dr. Afandi on May 15, 2024, advising that his actions constituted an unauthorized collection and use of PHI and inviting him to withdraw his reappointment application with the hospital.
Step 2 – Investigate
The hospital conducted an internal investigation and notified the Information and Privacy Commissioner (IPC).
Records showed that Dr. Afandi had completed Privacy, Security, and Confidentiality training in October 2020 and had signed a confidentiality agreement with WRH. He also confirmed he reviewed WRH’s privacy module again when he reapplied in April 2024.
Step 3 – Notify
The hospitals reported the breach to the IPC on May 31, 2024, and to the College of Physicians and Surgeons of Ontario on June 1, 2024.
Notification letters were sent to potentially affected families the week of July 2, 2024, describing the incident, the PHI involved, and corrective actions. A hotline was provided for questions.
Step 4 –Prevent the Breach from Happening Again
AMP powers to address a privacy breach signal a new era of active enforcement in Ontario’s health privacy landscape.
Administrative Monetary Penalties (AMPs) came into effect under PHIPA on January 1, 2024. This update to the legislation gives the Information and Privacy Commissioner (IPC) authority to issue AMPs of up to $50,000 for individuals and $500,000 for organizations in cases of PHIPA non-compliance.
In this case, the Commissioner exercised those new powers and fined:
- Dr. Afandi (individual) – $5,000
- WE Kidz Pediatrics (clinic as custodian) – $7,500
Both were penalized for unauthorized access and use of PHI for personal gain.
The IPC found that WE Kidz opened without a compliant privacy program — a key factor in the penalty decision.
WE Kidz was also required to complete privacy training and develop formal privacy policies and procedures. The Commissioner also recommended that WRH improve its record-keeping and monitoring to better demonstrate compliance in future audits.
Commissioner’s Investigation
The IPC emphasized the importance of “demonstrable accountability.”
“Demonstrable accountability” refers to a repeatable and evidence-based system of data governance whereby organizations can show regulators and individuals how they meet their legal and professional responsibilities in practice.
In the data regulatory context, the concept has evolved beyond basic checklist compliance. It now requires organizations to prove that their accountability mechanisms are active and effective — that safeguards are working as intended to reasonably protect personal health information.
In other words, demonstrable accountability means being able to measure, document, and demonstrate that privacy protections are in place, maintained, and effective — not just written in a policy.
Being able to demonstrate compliance is a regulatory expectation under PHIPA — and it’s the key to avoiding costly penalties.
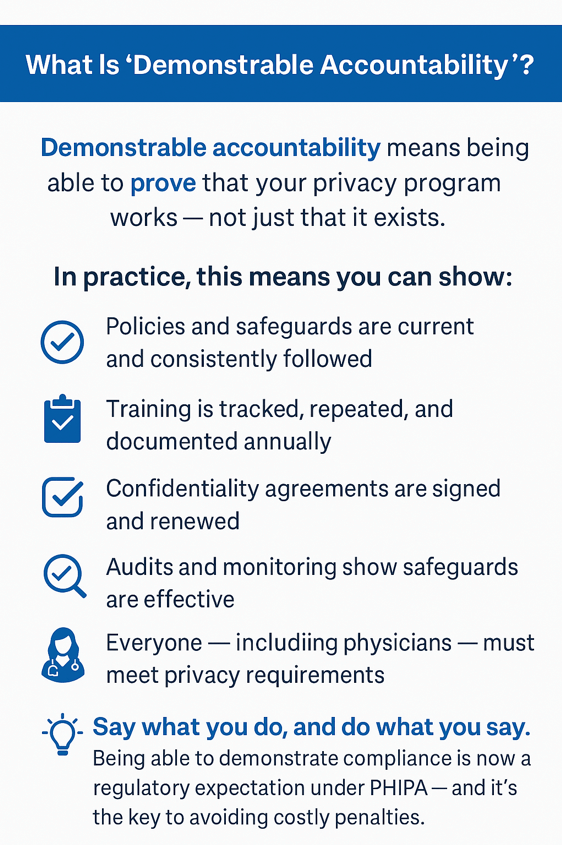
Under Section 10 of PHIPA, custodians must have information practices describing how they collect, use, disclose, retain, and safeguard PHI — and they must comply with those practices in day-to-day operations.
Take-Aways
✅ “Demonstrable accountability” means having evidence that your privacy program is working — not just written policies on a shelf.
✅ Maintain dated policies, training checklists, and signed confidentiality agreements for every team member.
✅ Replace “professional deference” with consistent expectations — all healthcare providers must complete privacy training and demonstrate understanding.
✅ Document and review your privacy program annually to ensure that safeguards and practices are effective in real life.
✅ Unauthorized secondary use of PHI — even for legitimate healthcare services — is a serious breach and can result in financial penalties.
Need Help Training Your Privacy Team?
Join the Practice Management Success Membership to access privacy awareness training, templates, and resources to strengthen your privacy management program.
Reference
Information Privacy Commissioner of Ontario. PHIPA Decision 298. August 28, 2025. https://www.ipc.on.ca/en/decisions/latest-decisions/phipa-decision-298
You May Also Be Interested In
Medical Secretary Fined for Unauthorized Access And Disclosure to Health Information